Kelly Flynn, SPT – Texas State University Doctorate of Physical Therapy Class of 2024
The title of this post is misleading to a certain degree. Is there a BEST choice for an ACL graft for knee reconstructive surgery? The answer is no, but there might be a best option for you, that is different from the next guy. Let’s look at the options and at surgical trends in recent years and decipher the benefits and risks of each graft. The popular available options for an ACL reconstruction graft are “Autografts” – meaning that the torn ligament is rebuilt using tissue from the patient’s own body, like the Hamstring tendon, Patellar tendon, or Quadriceps tendon. Another option is an “Allograft”, meaning donor tissue from a cadaver.
For starters, let’s look at the function of the ACL, and what tearing it entails. The main obligation of the Anterior Cruciate Ligament is to prevent anterior translation of your tibia on your femur. In other terms, it prevents your shin bone from moving too far forward in relation to your thigh bone. This ligament also provides proprioceptive feedback to your brain, meaning it helps tell your brain where your leg is in space. This feature helps with balance and stability of the knee joint. The common mechanism of injury for this ligament is in a non-contact event during a pivoting or cutting action, or while jumping with the knee slightly flexed in a valgus (“knocked-kneed”) position. This injury is very common in sports that involve cutting, jumping and rapid changes of direction.
So let’s say the unfortunate event of tearing your ACL has occurred… what now? The options are to either undergo non-operative treatment, meaning physical therapy to strengthen your knee joint and improve stability and balance, or have an ACL reconstruction surgery. Conservative treatment works well for some, especially persons who are described as “copers” whose criteria I have listed below:
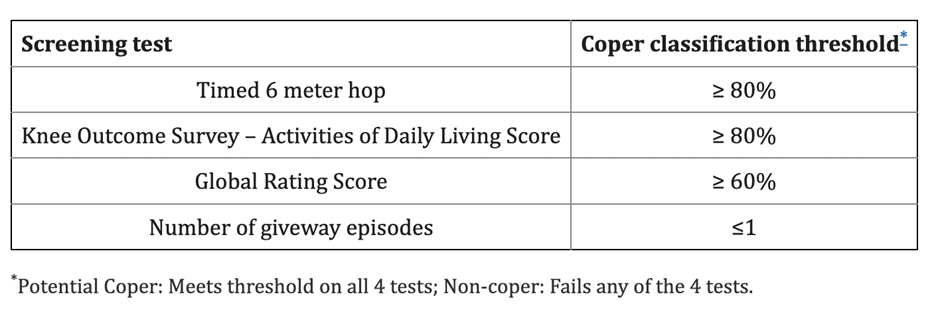
“Copers” are basically people who might be able to still have enough knee stability to accomplish all of their typical activities even without having their ACL intact. But not everyone fits these criteria, and some people have higher levels of typical physical demands – such as elite sporting activities or high-intensity labor functions on the job – which might make reconstructive surgery a better option. Interestingly, one study by Thoma et al found that patients who were classified as “Copers” were more likely to have a successful two-year outcome post-injury, as compared to non-copers – whether they underwent surgery or not.
Now let’s dive into the pros and cons of each ACL graft type. The Hamstring tendon graft typically uses the Semitendinosus and/or Gracilis tendons, bundled together and secured with a screw. These muscles are on the back side of the inner knee. The benefits of this graft are that it is from the patient’s own body, so it has a low risk of rejection and infection, and it is very strong, as it consists of two tendons bundled together to provide support to this graft. However, cons of this graft are that patients may also have adverse side effects of where the tendons were harvested, or cut, such as pain or weaker hamstring strength. These grafts hold up well overall, but when they fail, it is most commonly due to a secondary meniscal cartilage tear in the knee.
The Patellar tendon graft includes a bone graft taken from the patella to help facilitate stability and healing. The patellar tendon connects your kneecap to your shin bone. This type of graft has long been considered the “gold standard” of ACL reconstruction, because it typically holds up well. The possible problematic side effects of this graft are anterior knee pain during activity and/or pain with kneeling on the kneecap or the front of the knee – particularly in females. This graft most commonly fails due to a cyclops lesion, or scar tissue growth on the graft, that weakens its integrity and can lead to a tear.
The Quadriceps tendon graft includes two bundles of tissue, which is more identical than the other grafts to the native ACL structure. The Quadriceps tendon is located just above the kneecap and connects the quads muscles on the front of the thigh to the knee cap. This graft option is growing in popularity during recent years and has shown better results in comparison with other graft types in terms of decreased harvest site problems and/or pain, as well as a lower long-term graft failure rate. However, because of the relatively new widespread use of this graft, more research is needed to support the relative benefits and/or drawbacks of this type of procedure.
The Allograft is typically an Achilles tendon from a cadaver body. This graft has previously been observed to be associated with a higher rate of infection and as such is not recommended for pediatric and younger patients. However, current methods of harvesting and storing donor tissue have significantly decreased infection risk. The benefits of this graft type are that there is no harvest site morbidity or pain. For example, you won’t have weaker hamstrings or pain because they didn’t cut out a part of your hamstring tendon for the graft. Because this graft type involves less invasive surgical procedures, typically patients are able to resume typical daily activities much more quickly after surgery. However, a mildly longer wait is recommended compared to other graft types prior to returning to cutting and pivoting sport-type activities, because it takes longer for this type of tissue to fully rebuild than for other graft types. This longer healing time can stretch the return to full activity out by several months compared to the other reconstruction methods.
The Haybach et al. systematic review of 194 studies of ACL reconstruction results showed the yearly failure rate values of Hamstring tendon (1.70%), Patellar tendon (1.16%), Quadriceps tendon (0.72%), and allografts (1.76%). This is a good comparison, but it is important to note that these numbers are only after the first year of post-operative care. Some research indicates that it can take 2 years for any type of ACL graft to fully mature. One study by Runer et al found that the Hamstring Tendon was the most popular worldwide, followed by the patellar tendon, and then the quadriceps tendon. But it seems as though more surgeons are beginning to favor the Quadriceps Tendon, so these trends might change.
The summary of this comparison is that there are multiple options for post-injury care after sustaining an ACL tear. Whether or not you choose to undergo surgery, and what type of graft to use if surgery is planned, are individual choices that should be considered between you, your doctor, and your physical therapist.
Key Points:
- Ask your Physical therapist if you are a “Coper”.
- Communicate with your Surgeon and Physical Therapist about what graft type may be best for your individual circumstances.
- Research your surgeon and their individual preferences for surgical technique.
REFERENCES:
- Physiopedia contributors. Anterior Cruciate Ligament (ACL) Injury. Physiopedia. 2022. Accessed July 24, 2022.
- Dhammi, Ish Kumar, et al. “Graft Choices for Anterior Cruciate Ligament Reconstruction.” Indian Journal of Orthopaedics, Medknow Publications & Media Pvt Ltd, 2015,
- Thoma LM, Grindem H, Logerstedt D, et al. Coper classification early after anterior cruciate ligament rupture changes with progressive neuromuscular and strength training and is associated with 2-year success: The Delaware-Oslo ACL Cohort Study. The American Journal of Sports Medicine. 2019;47(4):807-814. doi:10.1177/0363546519825500
- Haybäck, Gerwin, et al. “Failure Rates of Common Grafts Used in ACL Reconstructions: A Systematic Review of Studies Published in the Last Decade.” Archives of Orthopaedic and Trauma Surgery, 2021, https://doi.org/10.1007/s00402-021-04147-w.
- Runer A, Keeling L, Wagala N, et al. Current trends in graft choice for Anterior Cruciate Ligament Reconstruction – part I: Anatomy, biomechanics, Graft incorporation and fixation. Journal of Experimental Orthopaedics. 2023;10(1). doi:10.1186/s40634-023-00600-4

