This post was written by Kyle Suh, SPT – Texas State University, Doctorate of Physical Therapy, Class of 2025
SCENARIO: Let’s say you are playing the game Scattergories and the category is Joints.
What joints would you list on your piece of paper?
Elbow? Shoulder? Knee? Hips?… probably about anything other than the jaw.
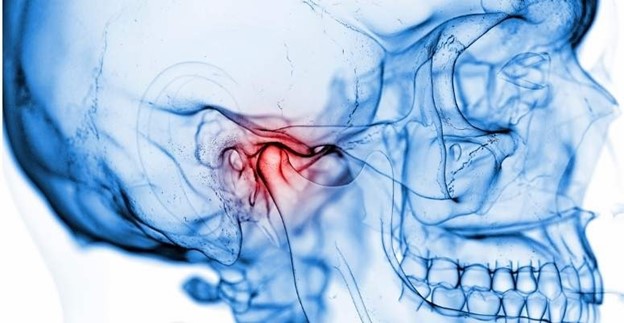
Understanding the TMJ and Dysfunction
The jaw, more specifically the temporomandibular joint (TMJ), functions as a joint in the same capacity as any others. The TMJ consists of muscles controlling motion, a surrounding capsule, and bones that articulate with one another. What differentiates treating TMJ dysfunction from that of knee or elbow? The answer: nothing at all.
Physical therapists are musculoskeletal specialists, and the TMJ falls under that system.
TMJ Dysfunction symptoms include, but are not limited to:[1]
- Pain or tenderness at the jaw and cheeks
- Popping, clicking during movement
- Limited range of motion or feeling of ‘getting stuck’
- Headaches, earaches, facial pain
- Pain while chewing, talking, yawning, etc.
TMJ dysfunction can greatly affect quality of life, affecting one’s ability to eat and speak. Additionally, jaw pain is often associated with facial pain, headaches, difficulty in concentration, and increased stress and anxiety. Despite the importance of the jaw in activities of daily living, it’s often overlooked and not immediately thought of as a valid candidate for physical therapy.
What can Physical Therapy Do?
It’s important to look at the person holistically, not just at the specific area of discomfort. TMJ dysfunction is multidimensional, the problem could arise from the joint itself, but it’s crucial to consider other contributing factors like: neck and back mobility, posture, soft tissue restrictions, and stress/anxiety/mental health.[2,3,4]
Everyone’s pain/discomfort is perceived differently. TMJ dysfunction does not necessarily have a black-and-white presentation. Understanding the uniqueness of dysfunction among different people, your physical therapist will analyze and provide an individualized evaluation and plan of care based on contributing factors to YOUR dysfunction.
Some things to expect, but not limited to:
Manual Therapy:
- Joint mobilizations: Techniques applied to the neck, back, or jaw to increase joint mobility
- Soft Tissue Mobilizations: Techniques to relieve muscular tension and improve mobility – including upper back and neck muscle release and/or intraoral (inside the mouth) jaw muscle release.
Therapeutic Exercises:
- Postural re-correction: Neuromuscular re-education focused on correcting posture to allow TMJ to function in its optimal position.
- Jaw exercises: Motor control of opening/closing, lateral deviation, and protrusion/retraction of jaw and the stabilizing muscles surrounding the TMJ.
- Mobility exercises: Exercise to increase range of motion of the jaw, neck, and back.
Education and Self-Management Strategies:
- Pain science education: Education regarding what may be contributing to the pain and how to effectively manage it
- Breathing techniques: Breathing strategies to help modulate stress/anxiety that could be contributing to muscular tension and TMJ dysfunction[4,5]
- Mental health resources: Provide resources or techniques to manage stress and other emotional factors due to the established relationship between mental health and TMJ dysfunction.[4]
Conclusion:
Research demonstrates the effectiveness of physical therapy in managing TMJ dysfunction. The jaw is a joint just like any other and physical therapists would treat TMJ the same way they would with an elbow or knee.
If you are experiencing jaw pain/discomfort, physical therapy may be the answer. Physical therapists have a good understanding of the multifaceted nature of TMJ dysfunction and its impact on everyday activities. Physical therapists can create an individualized plan of care for you and function as a guide for you on your path to pain relief and improved quality of life! If you have any questions about how therapy can help you, call your physical therapist today. They will likely be able to help and guide you!
References:
- GUIDE: Physical therapy guide to temporomandibular joint disorder. Choose PT. July 29, 2022. Accessed August 4, 2024. https://www.choosept.com/guide/physical-therapyguide-temporomandibular-joint-disorder
- Crăciun MD, Geman O, Leuciuc FV, Holubiac IŞ, Gheorghiţă D, Filip F. Effectiveness of physiotherapy in the treatment of temporomandibular joint dysfunction and the relationship with cervical spine. MDPI. November 17, 2022. Accessed August 4, 2024.
- Okeson JP. Temporomandibular disorders: Etiology and classification. SpringerLink.
January 1, 1970. Accessed August 4, 2024.
- Koray ORAL, Burcu BAL KÜÇÜK, Buğçe EBEOĞLU, Sibel DİNÇER. Etiology of temporomandibular disorder pain – journalagent. Accessed August 5, 2024. http://jag.journalagent.com/agri/pdfs/AGRI_21_3_89_94.pdf.
- Perciavalle V, Blandini M, Fecarotta P, et al. The role of deep breathing on stress – neurological sciences. SpringerLink. December 19, 2016. Accessed August 4, 2024. https://link.springer.com/article/10.1007/s10072-016-2790-8?correlationId=8806e3e97c91-4807-8462-792e593fc8a9&error=cookies_not_supported&code=daa444bd-df804b1e-b724-79afe9d38c99.